Rep. Buddy Carter:
“You have the insurance company that owns the PBM, that owns the group purchasing organization that owns the pharmacy, that owns the doctor.”
Simone Del Rosario:
Those days could be numbered if Senators Elizabeth Warren and Josh Hawley get their way.
The two sponsored a bill that forces companies that own health insurers or pharmacy benefit managers to sell off their pharmacy business.
The world of medicine has become increasingly incestuous. And PBMs are in the middle of it all.
“I’m sorry, this medicine isn’t covered by your insurance.”
“Yeah… I decide which medicines you can get.”
“Wait, you’re not my doctor.”
“That’s right. I’m your insurance company’s Pharmacy Benefit Manager or PBM.”
“And I don’t make that much money off this one.”
Wendell Potter:
A pharmacy benefit manager is, once again, it’s a middleman between a drug manufacturer and the pharmacy and ultimately to the patient who needs the medication. And insurance companies used to just hire them or use them to access the medicines be kind of their consultant, if you will
I’m Wendell Potter. I’m a former health insurance company executive. I left that career after a crisis of conscience, and I’ve been a health care reform advocate ever since, and even a whistle blower.
Simone Del Rosario:
Potter, who served as an executive with Cigna, details how twisted consolidation has become in recent years, with pharmacies getting the short end of the stick.
Wendell Potter:
CVS owns, or has owned, you’re right. They’re closing some of their retail establishments, about 10,000 stores, and they own Aetna, which is one of the very biggest health insurance companies, but the PBM, which is called Caremark, actually generates more revenue and more profit than those 10,000 stores or the Aetna health plans.
United Health Group, the biggest insurance company out there. It’s the fifth largest company in America on the Forbes list of American companies. CVS is right behind it number six.
And at a UnitedHealth Group, Optum is the division that houses its PBM, which is called Optum RX, and it now, just this year, is generating more revenue and profits for the parent company, UnitedHealth than the health plan side.
Simone Del Rosario:
Each of these companies offers a way to fill prescriptions, including via mail-order. But the Wall Street Journal pointed out this summer that mail-order drugs are often more expensive.
“PBMs have manipulated the market to enrich themselves — hiking up drug costs, cheating employers, and driving small pharmacies out of business,” Warren said in a statement.
Hawley added, “This legislation will stop the insurance companies and PBMs from gobbling up even more of American health care and charging American families more and more for less.”
The PBM trade group, Pharmaceutical Care Management Association, said in a statement, “This proposed legislation would severely limit access to safe and affordable pharmacies that patients value and rely on for prescription drugs. The truth is PBM-affiliated pharmacies, including mail-service and specialty pharmacies, have a proven track record of providing convenient, reliable, and affordable options for patients to access prescription drugs.”
In a survey commissioned by PCMA, 90% of responding employers “expressed satisfaction with their PBMs’ clarity and transparency of contract terms,” while 88% “expressed satisfaction with their PBMs’ ability to provide the lowest costs for employees at the pharmacy counter.”
PCMA has said Congress should focus on the “real way” to lower the cost of prescription drugs: holding Big Pharma accountable.
Straight Arrow News requested an on-camera interview with PCMA for ongoing coverage on PBMs. The trade group never responded to our request.
Warren and Hawley’s Patients Before Monopolies Act would restrict a parent company of a PBM or an insurer from owning a pharmacy business. It would also require anyone who is in violation of the law to divest the pharmacy business within three years.
Rep. Buddy Carter:
first of all, you have patient steering, where the PBMs the insurance companies are steering their patients toward their pharmacy, and they reimburse their pharmacies more than they reimburse independent retail pharmacies. Secondly, you know, there are oftentimes when the independent retail pharmacy can’t even participate, can’t even service the patient, and that, of course, is wrong
I’m Buddy Carter. I’m the congressman from the first Congressional District of Georgia, and a pharmacist by profession and have been serving in Congress now for 10 years.
“I started practicing pharmacy way back in 1980 and, you know, PBMs really started out as being nothing but processing. They just process claims. And all of a sudden, formularies became very prevalent, and in hospital settings and in other ways, and insurance companies began to understand that they could influence the price of a the price of a medication by including them on their primary on their formulary.”
Simone Del Rosario:
A formulary is essentially a list of prescription drugs covered by an insurance plan.
Wendell Potter:
These companies ultimately saw that there would be a way for them to make excess profits by owning these pharmacy benefit managers. So that’s what they did. CVS, bought caremark several years ago. Cigna, where I used to work, bought Express Scripts in 2018 and it is now much bigger than the health insurance part of Cigna. So Cigna now more is more is more apt to be described as a PBM or pharmacy benefit manager that also happens to own health insurance plans or operate health insurance plans is an entirely different company.
Simone Del Rosario:
Congressman Carter has been a vocal critic of PBMs for many years.
Rep. Buddy Carter:
I practiced pharmacy for over 40 years, and I was the one who had to go to the counter and tell the patient how much their medication was. I was the one who watched a senior citizen try to make a decision between buying groceries and buying drugs. I was the one who had to tell the mother how much her child’s antibiotic was and watch her in tears she’s tried to figure out how to how to pay for it.
Simone Del Rosario:
No insurance company should own a PBM, no PBM should own a pharmacy. It’s a direct conflict of interest. We need competition in the marketplace.
Earlier this year, the FTC released an interim report on the effect PBMs have on the price of prescription drugs. That report found the “Big 3” PBMs, all owned by health insurance companies, control around 80% of prescription drug claims for 270 million people.
The largest among them, CVS Health, told Straight Arrow News, “Any policies that would limit our ability to negotiate with drugmakers and pharmacies would ultimately increase the cost of medicine in the United States.”
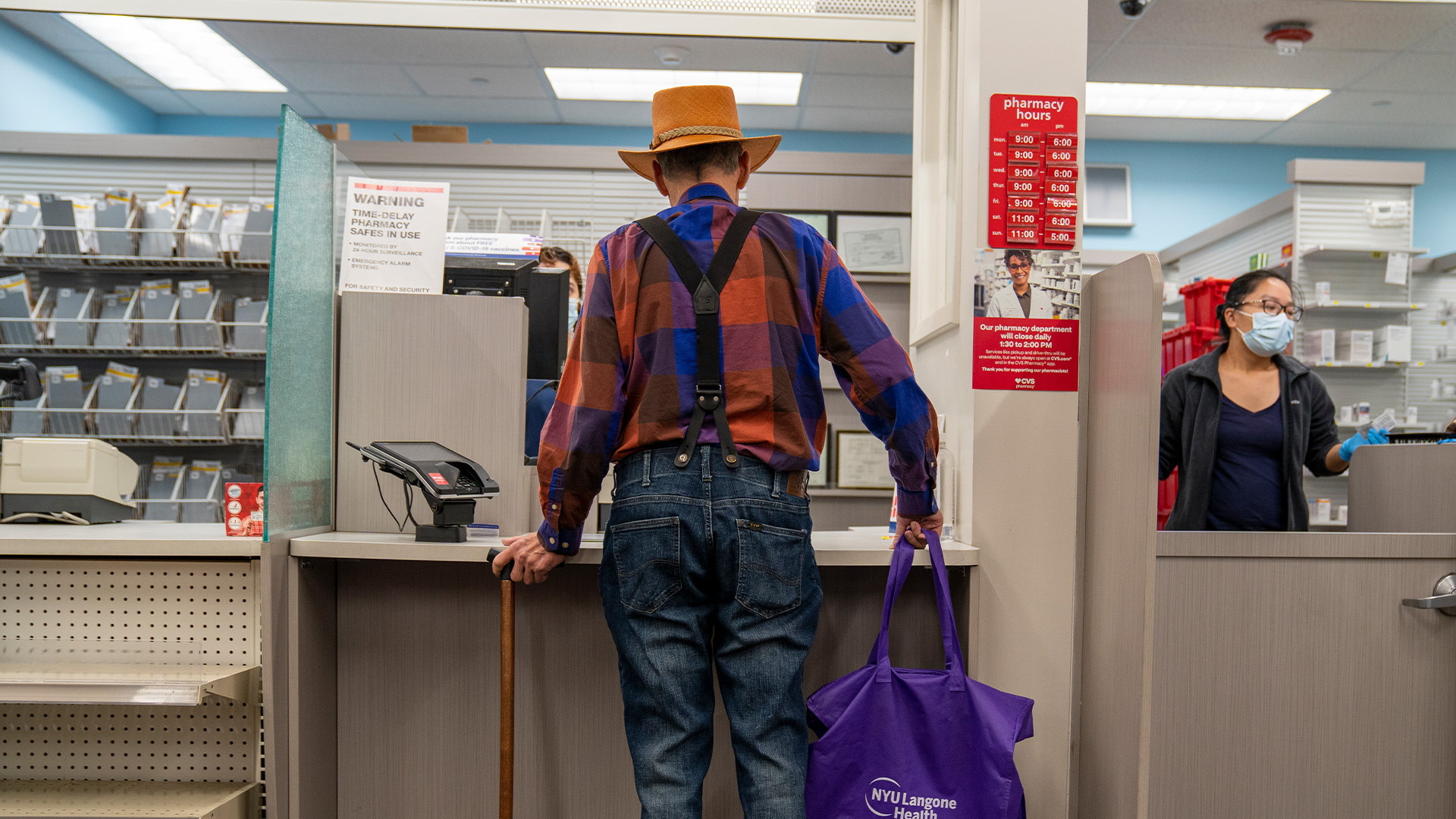
For many independent pharmacies, the cost of doing business is already too great.
John Hoeschen: | Owner, St. Paul Corner Drug
“If you pay $578 for something and you only take in $500, that’s not a sustainable model.”
Rep. Buddy Carter:
Last year, we lost 300 independent retail pharmacies, and we’re on page this year to lose one a day, almost 365 independent retail pharmacies
Even the largest pharmacies in the country are shutting down hundreds of stores this year. But in the case of CVS, they have their PBM and health insurance arms to fall back on.
Rep. Buddy Carter:
Look, pharmacists are the most accessible healthcare professionals in America. 95% of all Americans live within five miles of a pharmacy, but if we keep closing these pharmacies, particularly in the rural areas, that accessibility to health care is going to suffer. And you know, whether you’re Republican or Democrat or Independent, we all want the same thing. We want accessible, affordable, quality healthcare.
For continuing coverage on the plight of pharmacies, download the Straight Arrow News app and enable notifications.









